


UREA BREATH TEST
Breath Easy With CELIS
Accurate H.Pylori Diagnosis In Minutes

Breath Easy With CELIS
Accurate H.Pylori Diagnosis In Minutes
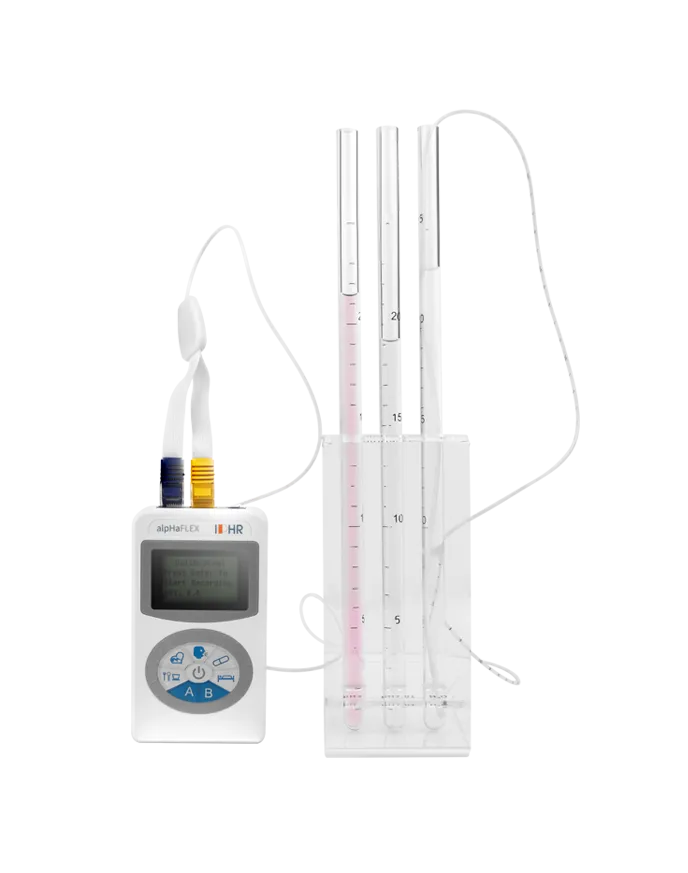
CELIS

Model: SUBT-D1
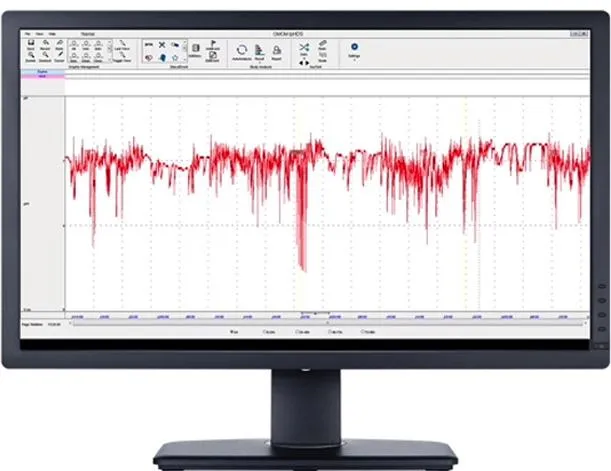
14C Urea Breath Test is used for primary diagnosis and post-treatment follow-up of H. pylori infections. The individual to be tested simply swallows 14C-urea. If H pylori presents, the enzyme urease produced by H pylori will metabolize 14C-urea to 14CO2 and ammonia. Then 14CO2 is transported in the blood to the lungs. When the patient exhales after a defined time this 14CO2 is captured in a breath collection card. No special preparation is needed before the analysis and since the UBT is both non-invasive, the method enjoys high acceptance.
Cut-Off Value
DPM ≤ 99, Negative
99 < DPM ≤ 149, the device will perform a second test automatically, and if it is still greater than 99, it’s positive
149 < DPM ≤ 499, Positive+
499 < DPM ≤ 1499, Positive ++
1499 < DPM ≤ 2499, Positive +++
DPM > 2499, Positive ++++
TESTING PROCEDURE
Take a capsule with empty stomach or 2 hours after eating.
Sit still for 15 minutes
Unpack the collection card and connect the mouthpiece to card body. Blow into breath collection card with appropriate force, you can exchange breath during blowing, but don’t draw in breath. Stop blowing when the card indicator turns from blue to white or after 3 mins even though color is not completely changed.
Give the collection card to medical staff and wait for report.

H PYLORI

Don't Ignore the Signs! Could You Have H. pylori?
Helicobacter pylori, a common bacterium, can infect the stomach lining and cause serious problems like ulcers and even cancer. It’s estimated that half the world’s population carries this bacteria. H. pylori spreads through person-to-person contact, often within families. If you’re diagnosed with H. pylori, it’s recommended that your close family members get tested and treated too.
H. pylori infection can cause a variety of digestive symptoms, such as bloating, nausea, vomiting, indigestion, burping, and loss of appetite. You may also experience more severe symptoms like dull or burning pain in the stomach, unplanned weight loss, and dark stools. It's important to note that these symptoms can vary in severity and may not always be present. If you experience any of these symptoms, it's recommended to consult a healthcare professional for diagnosis and treatment.
A significant medical advancement recognized that a specific bacteria, Helicobacter pylori, was responsible for a majority of duodenal ulcers and approximately two-thirds of gastric ulcers. This breakthrough earned a Nobel Prize. Nonsteroidal anti-inflammatory drugs (NSAIDs) and aspirin are known to cause most other peptic ulcers. When combined, H. pylori and NSAIDs can increase the risk of ulcers and bleeding. Eliminating H. pylori before starting long-term NSAID treatment can help reduce this risk.
H. pylori infection is estimated to increase an individual's lifetime risk of developing gastric cancer by 1.5 to 2%. However, early eradication of this bacteria, before the development of precancerous changes, has been shown to effectively prevent gastric cancer. This preventive measure is the foundation for widespread screening and treatment programs targeting young adults in regions with high rates of H. pylori infection and sufficient resources to implement such initiatives.
Indications for H. pylori Eradication:
1. History of ulcers: Duodenal or gastric ulcers, with or without complications
2. MALT lymphoma: A type of lymphoma associated with the stomach
3. Gastric mucosal abnormalities: Atrophy or intestinal metaplasia
4. Post-gastric cancer surgery: To reduce the risk of recurrence
5. Family history: First-degree relatives with gastric cancer
6. Patient preference: Based on consultation with their physician
7. Functional dyspepsia: Indigestion without a clear cause
8. NSAIDs: To prevent ulcers and bleeding in those not taking NSAIDs
9. Aspirin: To reduce the risk of ulcers and bleeding before or during long-term aspirin therapy
10. GERD: To support proton-pump inhibitor treatment
11. Cancer prevention: In areas with high gastric cancer rates
12. Blood disorders: Unexplained iron-deficiency anemia or idiopathic thrombocytopenic purpura
Note: This list provides a general overview of indications for H. pylori eradication. Specific recommendations may vary based on individual circumstances and healthcare guidelines.
The urea breath test (UBT) is the most widely studied and recommended non-invasive method for diagnosing H. pylori infection as part of a 'test-and-treat' approach. Monoclonal stool antigen tests (SAT) can also be used effectively. Serological tests, while viable, require careful validation. It's important to avoid using rapid, on-site serological tests with whole blood for H. pylori diagnosis.
CELIS

Model: SUBT-D1
14C Urea Breath Test is used for primary diagnosis and post-treatment follow-up of H. pylori infections. The individual to be tested simply swallows 14C-urea. If H pylori presents, the enzyme urease produced by H pylori will metabolize 14C-urea to 14CO2 and ammonia. Then 14CO2 is transported in the blood to the lungs. When the patient exhales after a defined time this 14CO2 is captured in a breath collection card. No special preparation is needed before the analysis and since the UBT is both non-invasive, the method enjoys high acceptance.
Cut-Off Value
DPM ≤ 99, Negative
99 < DPM ≤ 149, the device will perform a second test automatically, and if it is still greater than 99, it’s positive
149 < DPM ≤ 499, Positive+
499 < DPM ≤ 1499, Positive ++
1499 < DPM ≤ 2499, Positive +++
DPM > 2499, Positive ++++
TESTING PROCEDURE

Take a capsule with empty stomach or 2 hours after eating.
Sit still for 15 minutes
Unpack the collection card and connect the mouthpiece to card body. Blow into breath collection card with appropriate force, you can exchange breath during blowing, but don’t draw in breath. Stop blowing when the card indicator turns from blue to white or after 3 mins even though color is not completely changed.
Give the collection card to medical staff and wait for report.
H PYLORI

Don't Ignore the Signs! Could You Have H. pylori?
Helicobacter pylori, a common bacterium, can infect the stomach lining and cause serious problems like ulcers and even cancer. It’s estimated that half the world’s population carries this bacteria. H. pylori spreads through person-to-person contact, often within families. If you’re diagnosed with H. pylori, it’s recommended that your close family members get tested and treated too.
H. pylori infection can cause a variety of digestive symptoms, such as bloating, nausea, vomiting, indigestion, burping, and loss of appetite. You may also experience more severe symptoms like dull or burning pain in the stomach, unplanned weight loss, and dark stools. It's important to note that these symptoms can vary in severity and may not always be present. If you experience any of these symptoms, it's recommended to consult a healthcare professional for diagnosis and treatment.
A significant medical advancement recognized that a specific bacteria, Helicobacter pylori, was responsible for a majority of duodenal ulcers and approximately two-thirds of gastric ulcers. This breakthrough earned a Nobel Prize. Nonsteroidal anti-inflammatory drugs (NSAIDs) and aspirin are known to cause most other peptic ulcers. When combined, H. pylori and NSAIDs can increase the risk of ulcers and bleeding. Eliminating H. pylori before starting long-term NSAID treatment can help reduce this risk.
H. pylori infection is estimated to increase an individual's lifetime risk of developing gastric cancer by 1.5 to 2%. However, early eradication of this bacteria, before the development of precancerous changes, has been shown to effectively prevent gastric cancer. This preventive measure is the foundation for widespread screening and treatment programs targeting young adults in regions with high rates of H. pylori infection and sufficient resources to implement such initiatives.
Indications for H. pylori Eradication:
1. History of ulcers: Duodenal or gastric ulcers, with or without complications
2. MALT lymphoma: A type of lymphoma associated with the stomach
3. Gastric mucosal abnormalities: Atrophy or intestinal metaplasia
4. Post-gastric cancer surgery: To reduce the risk of recurrence
5. Family history: First-degree relatives with gastric cancer
6. Patient preference: Based on consultation with their physician
7. Functional dyspepsia: Indigestion without a clear cause
8. NSAIDs: To prevent ulcers and bleeding in those not taking NSAIDs
9. Aspirin: To reduce the risk of ulcers and bleeding before or during long-term aspirin therapy
10. GERD: To support proton-pump inhibitor treatment
11. Cancer prevention: In areas with high gastric cancer rates
12. Blood disorders: Unexplained iron-deficiency anemia or idiopathic thrombocytopenic purpura
Note: This list provides a general overview of indications for H. pylori eradication. Specific recommendations may vary based on individual circumstances and healthcare guidelines.
The urea breath test (UBT) is the most widely studied and recommended non-invasive method for diagnosing H. pylori infection as part of a 'test-and-treat' approach. Monoclonal stool antigen tests (SAT) can also be used effectively. Serological tests, while viable, require careful validation. It's important to avoid using rapid, on-site serological tests with whole blood for H. pylori diagnosis.
Capsule Endoscopy
Capsule Endoscopy

Reflux & Motility

Endoscopy Related

Omom Robotic





CONSUMABLES
Medical consumables in hospitals are essential items used in various medical procedures and environments to ensure patient safety and care. These include products like surgical gowns, drapes, and packs used to maintain a sterile environment during surgeries. Additionally, items such as masks, gloves, isolation gowns, and medical shoe covers are crucial for infection control and the protection of both patients and healthcare workers. Other consumables include medical aprons and devices that are regularly replaced to prevent contamination and support the effective functioning of medical and surgical procedures.
Hospital Bed Pillow Cases, 50×80cm,
Case of 200

Medical Shoe Covers

PP+CPE Shoe Covers

Disposable Surgical Cops

Hospital Bed Bed Covers

Disposable SMMS Standard
Surgical Gown SG019

Disposable Level 3 Full Reinforced
Surgical Gown

SMMS Reinforced Surgical
Gown - 30/Case

Wood pulp Spunlace Standard
Surgical Gown N73A00-4

Waterproof Disposable PP+PE Coated Polypropylene Coveralls
Get In Touch!
White Plains Block 57 Lot 09
Barangay Salu Porac Pampanga, Porac, Philippines
0905 230 6298
Signup our newsletter to get update information, news, insight or promotions.


Get in touch
White Plains Block 57 Lot 9 Brgy. Salu Porac, Pampanga Porac, Philippines
+63 0905 230 6298
Copyright 2024. KylledMed Philippines. All Rights Reserved.